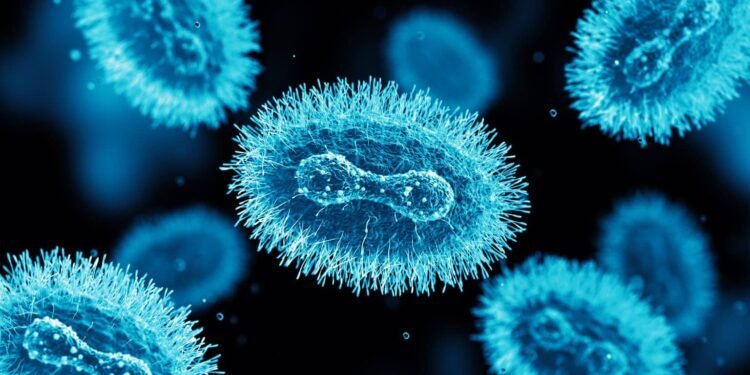
Mpox (formerly known as monkeypox) is a rare viral disease caused by the mpox virus, a member of the Orthopoxvirus genus, which also includes smallpox. While mpox is less severe and less contagious than smallpox, it can still cause serious illness in some individuals. Below is an overview of the disease:
1. History and Name Change
- Mpox was first identified in 1958in monkeys used for research, though the disease primarily occurs in rodents.
- The first human case was documented in the Democratic Republic of Congo (DRC)in 1970.
- In November 2022, the World Health Organization (WHO) announced the renaming of “monkeypox” to “mpox” to reduce stigma and inaccuracies in association with the disease.
2. Cause
- Mpox is caused by the mpox virus, which is an enveloped, double-stranded DNA virus.
- There are two distinct clades of the virus:
- Clade I(formerly Central African): More severe and transmissible.
- Clade II(formerly West African): Less severe and more common globally.
3. Transmission
- Mpox spreads through:
- Direct contactwith lesions, bodily fluids, or respiratory secretions of an infected person or animal.
- Fomites: Contaminated objects like bedding or clothing.
- Animal bites or scratchesfrom infected wildlife, particularly rodents and non-human primates.
- Human-to-human transmission can occur, particularly through close physical or intimate contact.
4. Symptoms
Symptoms typically appear 5–21 days after exposure and last 2–4 weeks. They include:
- Prodromal phase(early symptoms):
- Fever
- Headache
- Muscle aches
- Back pain
- Swollen lymph nodes (distinguishing feature from smallpox)
- Chills and fatigue
- Rash phase:
- Rash progresses through stages: macules → papules → vesicles → pustules → scabs.
- Lesions often appear on the face, hands, feet, and genitals but can spread to other areas.
5. Diagnosis
- Diagnosis is confirmed through laboratory tests:
- PCR (Polymerase Chain Reaction)testing of lesion samples is the most reliable.
- Blood tests or tissue samples can also detect the virus.
6. Treatment
- There is no specific treatment for mpox, but supportive care is essential:
- Antivirals:
- Tecovirimat (TPOXX)is approved for severe cases.
- Cidofovirand Brincidofovir may be used in certain cases.
- Pain management and hydration.
- Treating secondary bacterial infections if they occur.
- Antivirals:
- Vaccination with smallpox vaccines (e.g., Jynneos or ACAM2000) provides protection and can be used post-exposure.
7. Prevention
- Vaccination: The smallpox vaccine offers cross-protection due to the related nature of the viruses.
- Public health measures:
- Avoid close contact with infected individuals.
- Practice proper hand hygiene.
- Use protective equipment in healthcare settings.
- Education and awareness: Critical to controlling outbreaks.
8. Recent Outbreaks
- In 2022, there was a significant global outbreakof mpox, with cases reported in multiple countries where the disease was not endemic.
- This outbreak was linked to close physical and sexual contact, primarily affecting certain social networks.
- WHO declared mpox a Public Health Emergency of International Concern (PHEIC)in July 2022, which was lifted in May 2023 due to declining cases.
9. Endemic Regions
- Mpox is endemic in several Central and West African countries, including:
- Democratic Republic of Congo
- Nigeria
- Cameroon
- In these regions, contact with infected wildlife is a significant risk factor.
10. Key Public Health Concerns
- Stigma: The name “monkeypox” and its association with specific communities led to calls for renaming.
- Vaccine equity: Limited access to vaccines in endemic regions.
- Disease surveillance: Enhanced monitoring is essential to prevent future outbreaks.